THE SIGNS & SYMPTOMS OF LC-FAOD
LC-FAOD can be very serious. People diagnosed with LC-FAOD are at risk of developing severe symptoms that can be life-threatening.
Symptoms typically appear within a few hours of birth but can also appear later in life
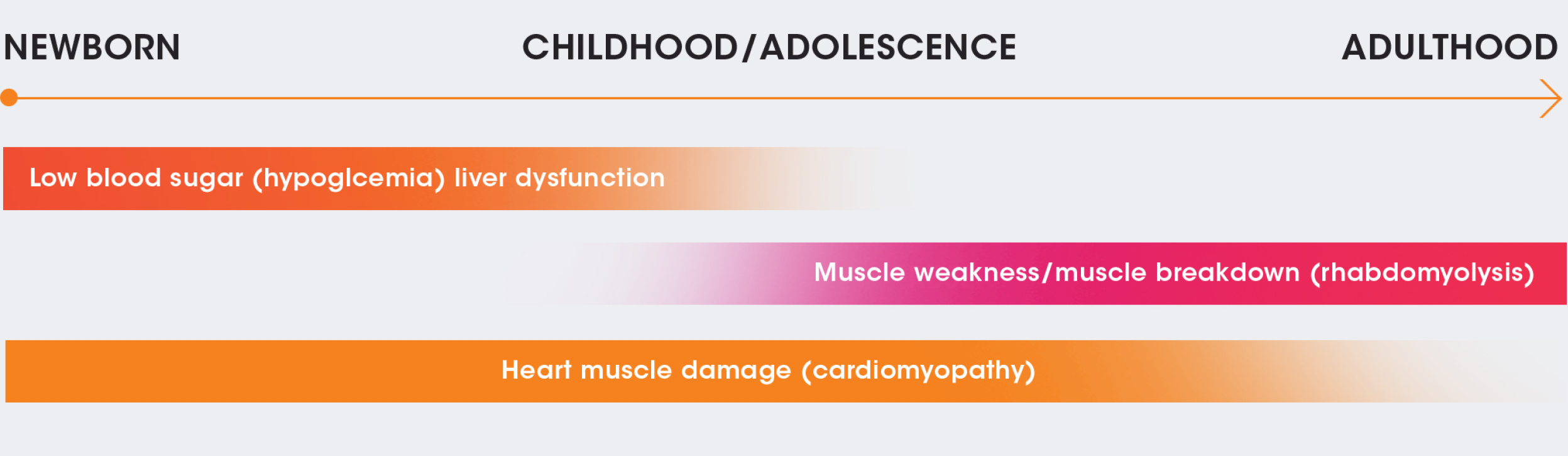
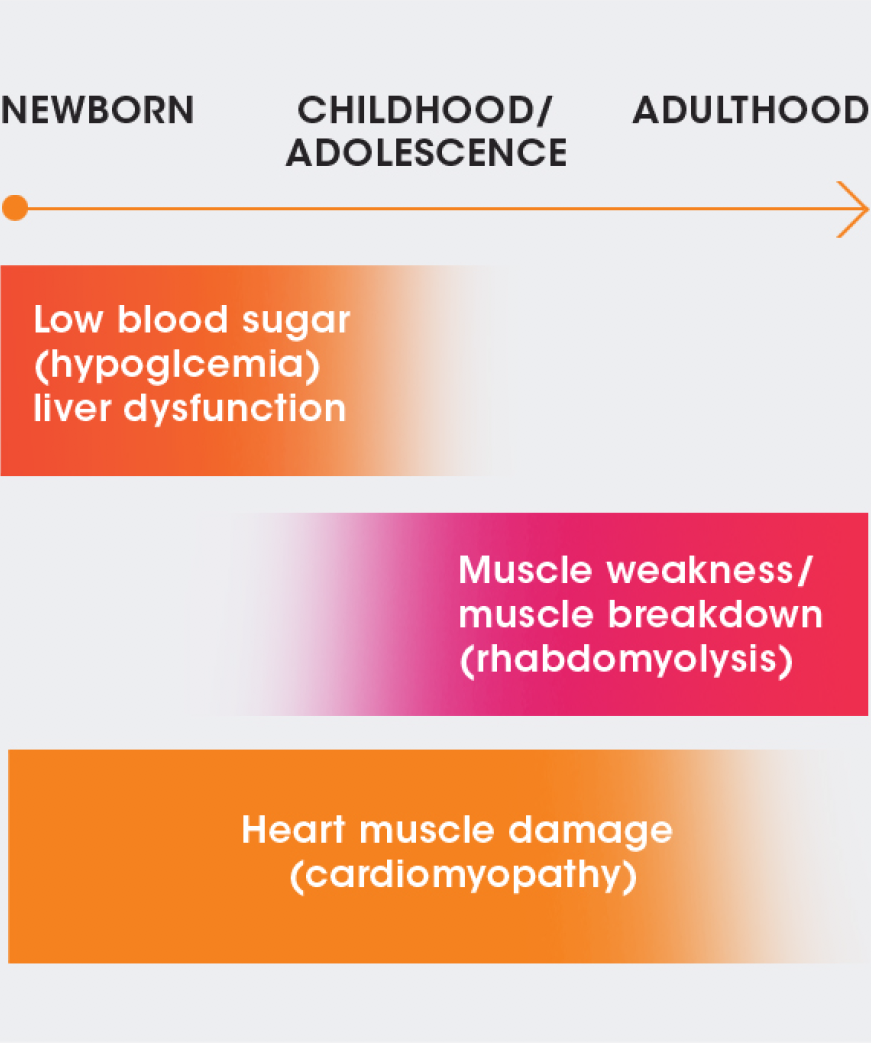
NEWBORN
CHILDHOOD/
ADOLESCENCE
ADULTHOOD
Low blood sugar (hypoglycemia)/liver dysfunction
Muscle weakness/muscle breakdown (rhabdomyolysis)
Heart muscle damage (cardiomyopathy)
Symptoms can come and go
These acute or episodic signs and symptoms of LC-FAOD develop suddenly; typically they occur during an illness or if you have skipped a meal, but they may also occur spontaneously or unpredictably. Acute metabolic crises may include serious conditions such as: chest pain†, muscle breakdown, nausea, stomach upset, appetite changes, or low blood sugar.
†May have a chronic impact.
Or they can be ongoing
Chronic (persistent or recurring) signs and symptoms develop, and may worsen, over time, and can include fatigue, muscle pain, muscle cramps, muscle weakness, and foggy thinking. These symptoms can be brought on or made worse by fasting or illness, sustained exercise, and physiologic stress and may lead to the following: decreased muscle tone, muscle pain or weakness, damage to the retina of eyes*, damage to nerves*, or liver dysfunction (hepatic dysfunction).
*Applies to certain LC-FAOD types such as LCHAD and TFP. Consult your healthcare provider for more information.
Symptoms can vary according to the LC-FAOD type
CPT I:
liver damage, elevated ammonia, low blood sugar with low ketones from birth to 18 months.
CACT:
low blood sugar with low ketones, high ammonia levels in blood, enlarged liver, heart muscle damage with or without irregular heartbeat, breathing difficulties, or muscle weakness in newborns and infants; milder symptoms with later onset.
CPT II:
elevated ammonia, low blood sugar with low ketones, heart muscle damage in newborns and infants; recurrent muscle breakdown in adolescents and young adults.
VLCAD:
low blood sugar with low ketones, high ammonia levels in blood in early childhood; recurrent muscle breakdown and myoglobin (an iron- and oxygen-binding protein) in the urine which causes kidney injury in adolescents and adults; and heart muscle damage at any age.
TFP:
low blood sugar with low ketones (similar to LCHAD deficiency but often more severe), high ammonia levels in blood in early childhood; severe nerve damage, retina damage at any age.
LCHAD:
low blood sugar with low ketones, high ammonia levels in blood in early childhood; recurrent muscle breakdown and myoglobin in the urine which causes kidney injury in adolescents and adults; skeletal muscle damage with or without recurrent muscle breakdown, nerve damage, retina damage at any age.
And there can be specific issues with children
Caregivers of babies and young children with LC-FAOD should watch for and be aware of symptoms of a metabolic crisis, including: neurologic distress (extreme sleepiness, coma, Reye’s syndrome), changes in heart beat, muscle weakness, or changes in appetite or dietary requirements. Keep a record and let your healthcare team know if you experience or observe any of these signs or symptoms.
A person’s quality of life may be substantially diminished as a result of LC-FAOD
With LC-FAOD, physical, mental, emotional, and social functioning can be negatively impacted. People can experience anxiety and depression due to continual avoidance of triggers (exercise, exposure to viral illness, cold or hot weather), fear of symptom recurrence or the long-term impact of LC-FAOD. If you are experiencing any of these issues, seek the help and guidance of a trained medical professional.
It impacts family and caregivers too
LC-FAOD demands families and caregivers to immediately establish and closely follow a specific diet and monitor physical activity. Care of individuals with LC-FAOD may require an around-the-clock commitment to check for signs and symptoms of deterioration and/or fatigue. The management of caloric intake, avoidance of fasting (including overnight), and potential monitoring/maintenance of enteral feeding tubes may result in restrictions on time and freedom.
